- About
- Topics
- Picks
- Audio
- Story
- In-Depth
- Opinion
- News
- Donate
- Signup for our newsletterOur Editors' Best Picks.Send
Read, Debate: Engage.
| July 26, 2022 | |
|---|---|
| topic: | Health and Sanitation |
| tags: | #Malaria, #health, #Africa, #Tanzania |
| located: | Tanzania |
| by: | Frank Odenthal |
The threat of malaria is far from over, and Africa remains the hardest hit continent. World Malaria Report 2021 finds that 95 percent of all malaria cases (approximately 228 million) occur in Africa. Of the 602,000 deaths from the disease, around 80 percent were children under the age of five.
FairPlanet spoke to Deus Ishengoma, principal research scientist, acting director and lab head at the National Institute for Medical Research (NIMR) in Dar es Salaam, about scientists' fight against malaria in Tanzania, one of the countries most affected by the disease.
FairPlanet: In your latest publication you highlight two major points of concern: that mosquitos are becoming resistant to the insecticides used on nets people surround their beds with, and that the parasites are developing immunity to the drug treatment based on Artemisinin combinations, which remains the only effective treatment for people who contract the disease. Can you elaborate?
Deus Ishengoma: So far, we have not been good at bringing on board new inventions and innovative methods of fighting malaria. Like the vaccines are yet to be depended on. The mosquitos are changing, because every organism tries to survive and reproduce to the next generation. They don‘t want to change because they want to continue to spread malaria - they want to survive. The same goes for the parasites as well. The more pressure you put on the organism, the organsim has to change. That is why mosquitoes are getting resistant to insecticides used in bed-nets and parasites are increasingly becoming resistant to the drugs we use to treat malaria. Otherwise, they would be eradicated.
So the situation for mosquito resistance is not getting under control; it‘s becoming increasingly worse. On top of that, in Africa, we‘re getting another type of mosquito that is difficult to deal with. It‘s currently invading the Horn of Africa, Ethiopia and Eritrea in particular, so the situation is going to worsen. That new mosquito provides a new malaria vector that is hard to deal with.
What about the parasite? Are treatments still up to the task of stopping it?
After we brought on treatments based on Artemisinin in the early 2000s, the so-called ACT (Artemisinin Combination Therapy), immediately resistance started to build up in Southeast Asia, in the Mekong region. And we‘ve already stated that if that would happen in Africa, the situation would be catastrophic.
The good thing, however, is that unlike in the past when treatments like chloroquine and other treatments before ACT became less useful and parasites that became resistant started spreading westwards from Southeast Asia to East Africa and further into the continent, resistance to ACT seems to be different. Instead of spreading, they are popping up in certain regions.
For the past ten years, we had no information about Artemisinin partial resistance until it was reported two years ago in Rwanda, last year in Uganda and this year in Eritrea. So in these three countries we have what is called 'Artemisinin partial resistance.' We call it partial resistance because it is resistant to one of the drugs inside the ACT, but the whole combination still seems to work for now.
So depending on the combination of the ACT, parasites are becoming more and more resistant. In Africa, we have not yet reported cases with full blown ACT resistance. In my team, we are currently doing research to monitor the emergence and spread of Artemisinin partial resistance in Tanzania. How these new parasites are spreading is currently not known, and the World Health Organization (WHO) is fighting hard to contain Artemisinin partial resistance in Africa. I‘m happy to be part of that initiative.
A resistance to Artemisinin-based treatments would truly be catastrophic for Africa, as it‘s still the only known effective treatment. Is that correct?
Yes. We have recently published our opinions and are saying the lights are yellow. and that at any time we could switch to red light, which would mean complete resistance to Artemisinins and ACTs. And that would be really bad in Africa.
Based on last year‘s report, one year of COVID-19 [let to] an increase of almost 40,000 deaths in Africa, and you can imagine the impact on our healthcare systems. So having Artemisinin resistance will be a disaster. We‘re are fighting for that not to happen, and currently we seem to be on top of things. I hope we will rescue the situation the same way it was done in Southeast Asia, where after they noted it, they pumped in different strategies and now the situation is, well, not fully but at least getting under control.
On top of that, detection of malaria in people reporting symptoms has now gotten more complicated as well…
Yes, in addition to the issues mentioned above - insecticide resistance in mosquitoes and drug resistance in parasites - we are now getting resistance against detection. It‘s catching us unaware and unprepared, and we have no idea how we should deal with it, because we know little about it.
Parasites are changing their DNA, chopping out the part of DNA that is responsible for making the protein that we are detecting in the blood, to the extent that it cannot produce that protein anymore. For us it‘s like we‘re losing the key, so we cannot open the door. That part of the DNA that has been chopped out is not vital for the parasite’s survival.
So when a patient comes into a hospital, and you can clearly see that he or she is sick, and the patient has parasites in the blood, but you cannot detect the parasites with the tests you are using unless you change to a different test. In so many areas of Africa where the economy is not good - trained experts are not there and there are no alternatives, these diagnostic tests have been very useful for malaria case management by supporting early diagnosis and treatment for the past ten years.
"The W.H.O is fighting hard to contain Artemisinin-partial resistance in Africa."
Are there any other ways to detect malaria in patients?
The most common, and old, method of finding the parasites in patients' blood is through the use of a microscope. This method was discovered in the late 19th century. It's about trying to magnify and see what is in the blood that you cannot see with naked eyes, and you are able to see the parasite and describe it.
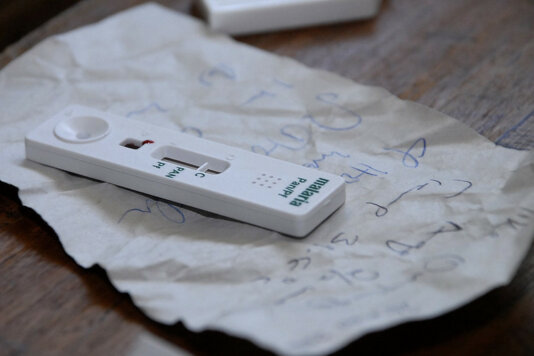
For malaria, until the late 1990s, about a hundred years later, it was the only method of detecting the parasite. In the 2000s, we started utilising parasite proteins that this parasite keeps producing and releasing into our blood once it enters our body. We could detect this protein in our blood through the then newly-developed rapid test kits. These tests are very easy to handle, unlike the method based on a microscope, which requires highly trained personnel, electricity and reagents.
Today in Tanzania, for example, less than ten percent of medical staff can properly detect the parasite using a microscope. So you have ninety percent of the staff employed in health facilities who cannot diagnose malaria very well. That's why the WHO says these rapid tests might have their limitations, but they are still much better than the microscope method which needs experts.
The rapid test kits were introduced in Tanzania in 2009 and finalised in 2012; millions of tests have been performed and millions of diagnoses have been made since. Their performance is between seventy to one hundred percent, but the thirty percent you lose is far better than maybe the ninety percent you lose when using a microscope.
What are the consequences of the parasite getting undetectable by these tests?
You know, Artemisinin combination therapy treatments are very expensive and pose a high risk of the parasite developing resistance. So if you use them on a patient who does not have malaria, you are spending almost ten dollars, and that‘s too much.
Imagine an average person who has maybe one or two dollars a day [to spend] and you are asking that person to buy a drug of ten dollars; it‘s inconceivable. So we saved a lot of drugs and actually delayed resistance in Africa, because since we started using that rapid tests the situation is that you cannot treat a negative patient. And that fits now into that diagnostic resistance, because when a patient has the parasite and tests come out negative, you can not treat! And if you cannot treat, you are denying drugs to a really sick patient. That‘s where we're getting stuck. And that‘s why we say this has do be dealt with as an urgent matter.
Are there alternative rapid tests at hand or currently being developed?
Alternative tests have been around, and they are good, but they are not easy to make, so they come with much higher costs. They are of little help for Africa, because quality controlled manufacturing is not guaranteed and they are far too expensive to be used on a large scale. Only a handful of companies currently produce them.
"Ninety percent of the staff employed in health facilities cannot diagnose malaria very well."
In your recent publication you recommend four elements that should be paid attention to when dealing with malaria in areas with or at high risk of having parasites that cannot be detected through rapid tests. The first recommendation is to further intensify surveillance. Can you explain why?
In order to tackle malaria, we need to know what the situation is in different areas. For example, in Tanzania we didn‘t know what was happening. We did the first study in 2017 as a follow-up to other two studies, but these were properly done as recommended by the World Health Organization.
Last year, we did our WHO-approved survey in 100 health facilities from 10 regions and recruited over 7,500 patients suspected to have malaria who attended the health facilities to get treatment. The preliminary results have shown that only 50 patients were suspected to have parasites that cannot be detected by the tests used in our country. We are finalising the laboratory analysis, but these results suggest that the situation is not that bad.
Knowing where the situation is bad or not bad is important for WHO and [governments] to be able to move forward and make a decision. For example, in Eritrea, it was observed that sixty to eighty percent of patients could not be detected by the [available] rapid tests, so they immediately changed to a different rapid test.
But, as I said, those alternative tests are too expensive to be used on a large scale. So in Tanzania we have this study now, and we will do an additional study next year and after that we will be able to come forward with policy recommendations.
The second recommendation is to monitor the development of rapid test kits.
Yes, if we would have alternatives of ten or more test kits, we would be able to switch and still be able to reliably detect malaria in patients. It‘s always better to have alternatives, especially when the situation changes quickly and is not properly overlooked. At the moment, we have no other choices, and that could prove fatal.
The third recommendation is to provide management guidelines to the specific regions afflicted with parasites that are resistant to rapid tests. What would those guidelines be?
Many countries, particularly in Africa, depend on WHO. They do less research and have limited technical exercise, so they can not sort themselves out. They need technical support, including guidelines and guidance from WHO. In Tanzania, for example, we just noted a few patients suspected of being undetectable, as mentioned above, so what should we do now to prevent and contain the spread of such new parasites? There is no clear guidance.
People who are out the in the field don‘t have the time to think about appropriate guidelines, they are focused on solving problems and need to act on the spot. These people need to be guided.
That’s why WHO and ministries of health need to ensure that their guidelines cover different situations and settings. This will guarantee that patients with malaria are promptly and properly detected and treated even in areas where diagnostic resistance has been confirmed and reported.
And the fourth recommendation is that all experts and research institutes act together, which sounds quite straightforward.
Solving such a big problem cannot be done by just one person. Everyone dealing with malaria needs to be aware of the problem and work towards preventing the emergence and spread of diagnostic resistances.
The more people we get on board with their respective experience in their respective country or region or scientific background, the better for all of us.
Dr Deus Ishengoma is Principal Research Scientist at the National Institute for Medical Research (NIMR) in Dar es Salaam, Tanzania. His research interests include genetic epidemiology of malaria, antimalarial drug resistance and the genomic basis of human susceptibility and/or resistance to malaria.
He completed his PhD in medical parasitology at the University of Copenhagen in 2011 and he is currently leading a country-wide surveillance of malaria in Tanzania using molecular methods.
Ishengoma is a member of the Pathogen Diversity Network Africa (PDNA) and a 2019 recipient of the Allan J. Magill Fellowship of the American Society of Tropical Medicine and Hygiene.
Image by Rick Scavetta, US Army Africa.
By copying the embed code below, you agree to adhere to our republishing guidelines.